Researchers in Delft and Leiden are working together to develop an implantable electronic ear. In the process, technological innovation is coming up against medical diligence.
The ear is such a delicate organ that even the most meticulous microsurgery may not be precise enough to restore hearing, explains Johan Frijns, Professor of Otorhinolaryngology at Leiden University. The ear is his favourite organ because of its physical complexity, neural sophistication, and its crucial role in human communication.
And because he is in a position to actually do something when a child is born deaf. Before the child’s first birthday, an implant is inserted into the cochlea (‘snail shell’) of the inner ear. Combined with an external electronic unit, this enables the child to hear and learn to speak.
Frijns told his parents that he wanted to study medical technology when he was sixteen. The medical aspect attracted him because it was useful, and technology because it was fun. The only problem was that such courses did not yet exist. So Frijns began by studying physics in Delft, and in his final year he started a degree in medicine at Leiden. He completed the second degree programme too, followed by a five-year specialisation in Otorhinolaryngology (Ear,Nose and Throat) In 2005 he was appointed professor in that field, and no-one will be surprised that, together with his colleague, clinical physicist and audiologist Dr Jeroen Briaire (also a Delft alumnus), he is extremely interested in new technologies that will benefit patients in the future.
‘Really weird things’
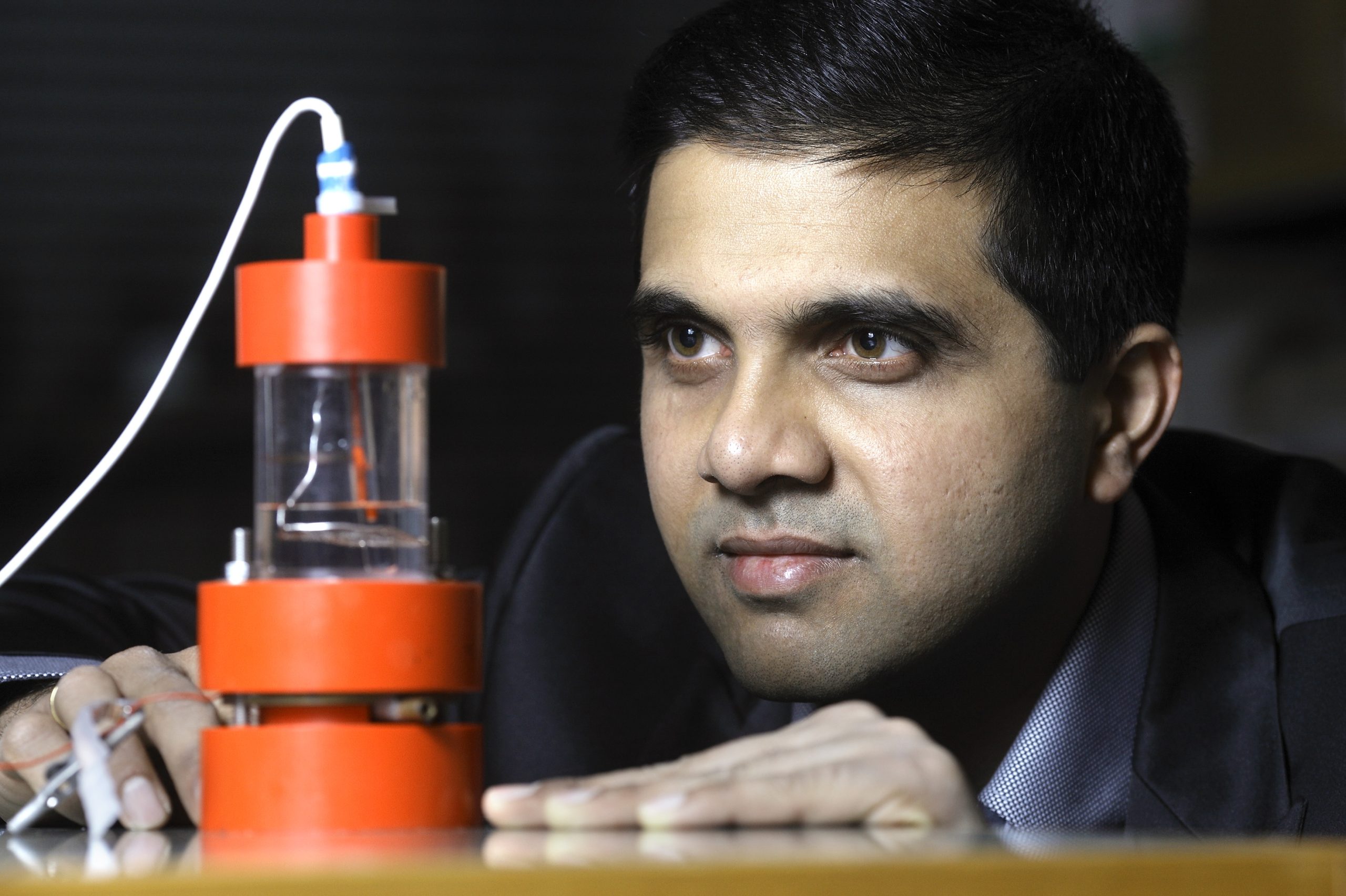
The Leiden ENT group is working with, among others, Prof. Paddy French, Nishant Lawand MSc. and Dr Wouter Serdijn of the Faculty of Electrical Engineering, Mathematics and Computer Science in the STW Perspective programme Smac-it (Smart Cochlear Implants),in which the American company Advanced Bionics is also involved. Paddy Boyle, Director of External Research at AB: “Officially, my job involves facilitating research in hospitals and universities. But in practice that comes down to telling our directors why they should support particular examples of academic research rather than the topics they have thought of themselves.” Boyle, who has quite a bit in common with professor of microelectronics Paddy French, sharing the same first name and Irish roots, finds university research interesting because of the ‘really weird things’ it produces, such as the silicon electrodes that Delft researchers are working on.
As mentioned above, the ear is a refined organ that nanotechnologists can learn quite a bit from. Frijns summarises how the ear works. Eardrum vibrations are transmitted via the familiar trio of bones(the ‘hammer’, ‘anvil’ and ‘stirrup’) to the twenty-times-smaller oval window of the fluid-filled cochlea. In this way, vibrations in the air are efficiently converted into vibrations in the fluid inside the cochlea. The remarkable thing about the inner ear is that it can distinguish frequencies. A real-time mechanical Fourier analysis takes place; each part of the membrane in the cochlea resonates to a certain frequency. The lower part of the cochlea resonates to the higher frequencies, and the upper part resonates to the lower frequencies. One octave corresponds to a distance of three millimetres. In total, the cochlea winds 2¾ turns. Some 3,000 hair cells transmit the vibrations to 30,000 neurons which, as a one-millimetre thick cochlear nerve, carry the information to the brain. Ten neurons per hair cell make it possible to distinguish subtle differences in sound strength for each pitch.
Bilaterally deaf
In some cases, however, something goes wrong at the development stage, and a child is born bilaterally deaf. In Netherlands this occurs in one in a thousand children, i.e. around 200 babies per year. Unable to hear anything and unable to learn to speak; it is difficult to exaggerate the difficulty of being excluded from spoken communication. But even in these children, the auditory nerve usually functions to some degree;
hence the idea to stimulate the acoustic nerve electronically. In 1957 this was done for the first time by a French ENT specialist and an engineer. The patient, a 50-year-old man who had become completely deaf as a result of previous operations, was given an implant with two thousand windings and stainless steel contacts. The signal was transmitted by an external coil. It may have been primitive, but the implant worked: the man could hear sounds, but initially he could not distinguish speech.
Modern implants consist of an external unit behind the ear that captures sound and splits it into between 8 and 120 channels with different frequencies. The unit feeds a coil with a magnet placed outside the skull opposite an implanted receiver. A wire connects the receiver to a row of electrodes (between 12 and 22) implanted inside the cochlea. Ninety percent of adult patients with this type of implant are able to hold a telephone conversation again.
But parties are something to be avoided, and music is also unpleasant for implant patients. The reconstructed hearing is but a shadow of what we normally experience as sound.
Acoustic simulations carried out with a voice encoder clearly demonstrate what a patient can hear after a cochlear implant: a ‘flat’, electrical scraping sound that stops suddenly and begins again. Depending on the number of channels the patient can decipher spoken text with varying degrees of difficulty – provided there is not too much background noise. Music can’t be enjoyed if guitar music sounds like an African drum concert.
Although the cochlear implant (or ‘bionic ear’) is a miracle of modern technology that has enabled a quarter of a million people to hear, there is clearly a great deal of room for improvement.
Reduced costs
Currently implants are made by hand, by women in the United States who have received 6 months’ training – at least, that is the case at Advanced Bionics. And the situation at the companies Cochlear (Australia) and MedEl (Austria)is probably similar. The women solder delicate insulated wires to platinum plates that are 0.3 x 0.4 millimetres in size. An implant 28 millimetres in length includes 16 of these in a row. This is a day’s work for one of these women, and the cost price for the electrodes is around 600 euros. It is not surprising that the 17-thread cable is somewhat rigid.
In Delft they have come up with a solution to this: with microelectronics technology it is possible to produce contacts industrially so that the electrodes can be standardised at a much lower cost.
The underlying problem is that existing implants are too cumbersome for the structure of the inner ear. It appears that the electrodes activate more than one hair cell, which means that the sound quality for the patient is worse than one would expect, given the number of channels and electrodes.
PhD student Nishant Lawand shows how the conductors and contacts can be built up layer by layer on a silicone wafer with a 10-micrometre thin layer of polyimide (a plastic-like material that is not toxic and will not be rejected by the body). When all the layers are in place, the silicon wafer is removed, leaving an extremely flexible strip of contacts – the electrode array. So far, the prototype has twelve contacts and thirteen guide tracks (one shared earth contact). It is 10 millimetres long by 1 mm wide.
Guinea pigs
Next year, Frijns plans to implant the prototype in guinea pigs. These animals are preferred by audiologists because the cochlea is easily accessible in the middle ear and is not embedded deep in the petrous part of the temporal bone. Together with Dr Wouter Serdijn (EEMCS), Frijns and Briaire are working on the STW project ‘ReaSONS’ (Realtime Sensing of Neural Signals). The aim of the researchers is not only to stimulate the inner ear, but also to measure the resulting neural signal, which is 100 to 1,000 times weaker.
They will study not only how the implant functions, but also how the body responds to it and vice versa. The human body appears to tolerate polyimide, but what about the titanium nitride that the contacts are made of? Will the components slowly disintegrate in the body? It is a fact that salt water damages electronics. How can this be prevented in the body?
Paddy Boyle sees the electrode array as a platform for innovation. The electronics boys want to be able to incorporate active elements in their strip. This will make it possible to increase the number of contacts to, say, two hundred, and still use only three wires (feed, earth and multiplex) to transmit signals to all the contacts.
An implant that is so thin and narrow is likely to adhere more closely to the inner surface of the cochlea, making it possible to stimulate smaller, more specific groups of neurons. The delicacy could make it possible to penetrate further into the cochlea, and hence control lower frequencies. The main advantage of the future electrode array appears to be the flexibility of control. After implantation, using the software, the audiologist can help the patient to find the best configuration of frequency channels and contacts. This configuration can subsequently be adjusted.
And the innovation doesn’t stop there: the researchers have also developed a 0.2 millimetre-square chip that can control the thin electrodes, as well as software for transmitting data through the skull in a more reliable and energy-saving way.
Frijns is aware that innovation in medicine is a long process. He estimates that it will be another ten years before he is given permission for a clinical trial with the first implants. “I hope it happens before I retire”, jokes the 50-year-old.
Frijns really appreciates the fact that he has access to the latest technology, and notices how Delft researchers enjoy working on concrete medical applications. The collaboration enables Frijns to ‘keep in step’ and ensure that he doesn’t develop solutions that are unusable (e.g. due to medical legislation).
“Medical specialists don’t tend to think outside their field. Technologists, on the other hand, can be so driven that they lose sight of applicability”, observes the physician/engineer.
 Which staff at Delft are involved in the research?
Which staff at Delft are involved in the research?Which staff at Delft are involved in the research?
– Smac-It project (funded by the STW technology foundation):
– Electrodes: Prof. Paddy French and Nishant Lawand MSc.
– Electronics: Dr Wouter Serdijn, Wannaya Ngamkham MSc and Chutham Sawigun MSc.
– Microcomputer: Dr Georgi Gaydadjiev and Ghazaleh Nazarian MSc.
– Reasons’ project (funded by the STW technology foundation):
– Electronics: Dr Wouter Serdijn, ir. Cees-Jeroen Bes and Yongjia Li MSc.



Comments are closed.